
When you think of acupuncture, it’s very likely that the first thing you think of is “needles.” And needles don’t necessarily evoke the most joyful memories (after all, who actually likes to get pricked?). In that case, you’re probably not rushing to be first in line to get dozens of needles in your body.
Ah, but that is where you’re wrong. You should be sprinting to be first in line to receive this ancient form of Chinese medicine. With just some paper-thin needles placed in strategic points on your body, you can improve your sleeping habits, your mood, and your allergies, and reduce pain and digestive issues.
Acupuncture is safe and effective, and relatively pain-free (it won’t hurt, but you will feel some sensation). You can use acupuncture to treat dozens of disorders or discomforts, but here are five of the most common reasons you should try it:
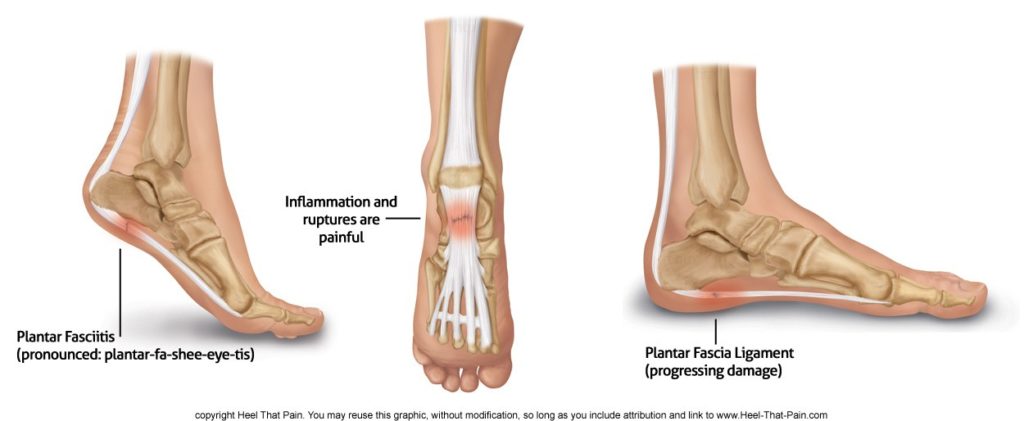
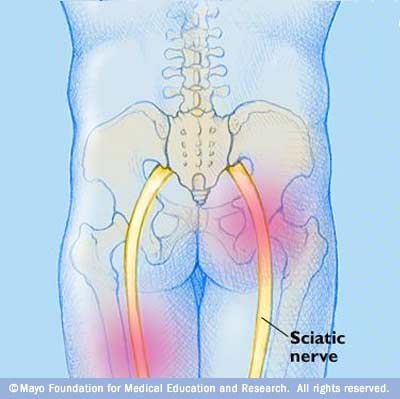
Soothe chronic pain: Acupuncture can reduce back pain, headaches, neck pain, and postoperative pain – basically any and all pains. Acupuncture is effective in its healing capabilities because the method is so personalized; it all depends on you and your body, and no two patients receive the same treatment for the same discomfort.
Improve sleep: According to the University of Maryland Medical Center, some reports suggest that certain acupuncture procedures have a nearly 90% success rate for treating insomnia. Other clinical studies have found that using needles placed at various points in the ear is effective in helping you fall asleep and stay asleep.
Alleviate digestive problems: Certain acupuncture points on the body are known to reduce abdominal pain and bloating, and regulate the overall digestive function. Researchers believe that acupuncture can prompt a decrease in stomach acid and speed up digestion, so less acid backs up into the esophagus.
Decrease seasonal allergies: If you are plagued with seasonal allergies, like sneezing and itchy eyes, acupuncture may help reduce the symptoms and lessen the amount of antihistamines you need. A recent study found that allergy patients who received acupuncture treatments showed a greater improvement in symptoms than those who didn’t use acupuncture.
Reduce stress: In Chinese medicine, stress and anxiety interrupt the energy flow in our bodies, causing tension in certain areas. Acupuncture addresses these “energy blockages” and works to alleviate stress by releasing endorphins and improving circulation throughout the body.
Acupuncture will change the way you think about needles. You won’t be scared of them anymore; instead, you will discover the amazing health and wellness benefits they can provide. Try it for yourself at Dreamclinic and book an acupuncture appointment today.
photo credit: http://media-cache-ak0.pinimg.com/736x/3b/53/b2/3b53b21ec48a85e7bb3504da79248e2e.jpg



 dy doesn’t seem like the most fun way to treat ailments, acupuncture is a tried and true therapeutic practice that has helped people deal with pain for centuries.
dy doesn’t seem like the most fun way to treat ailments, acupuncture is a tried and true therapeutic practice that has helped people deal with pain for centuries.